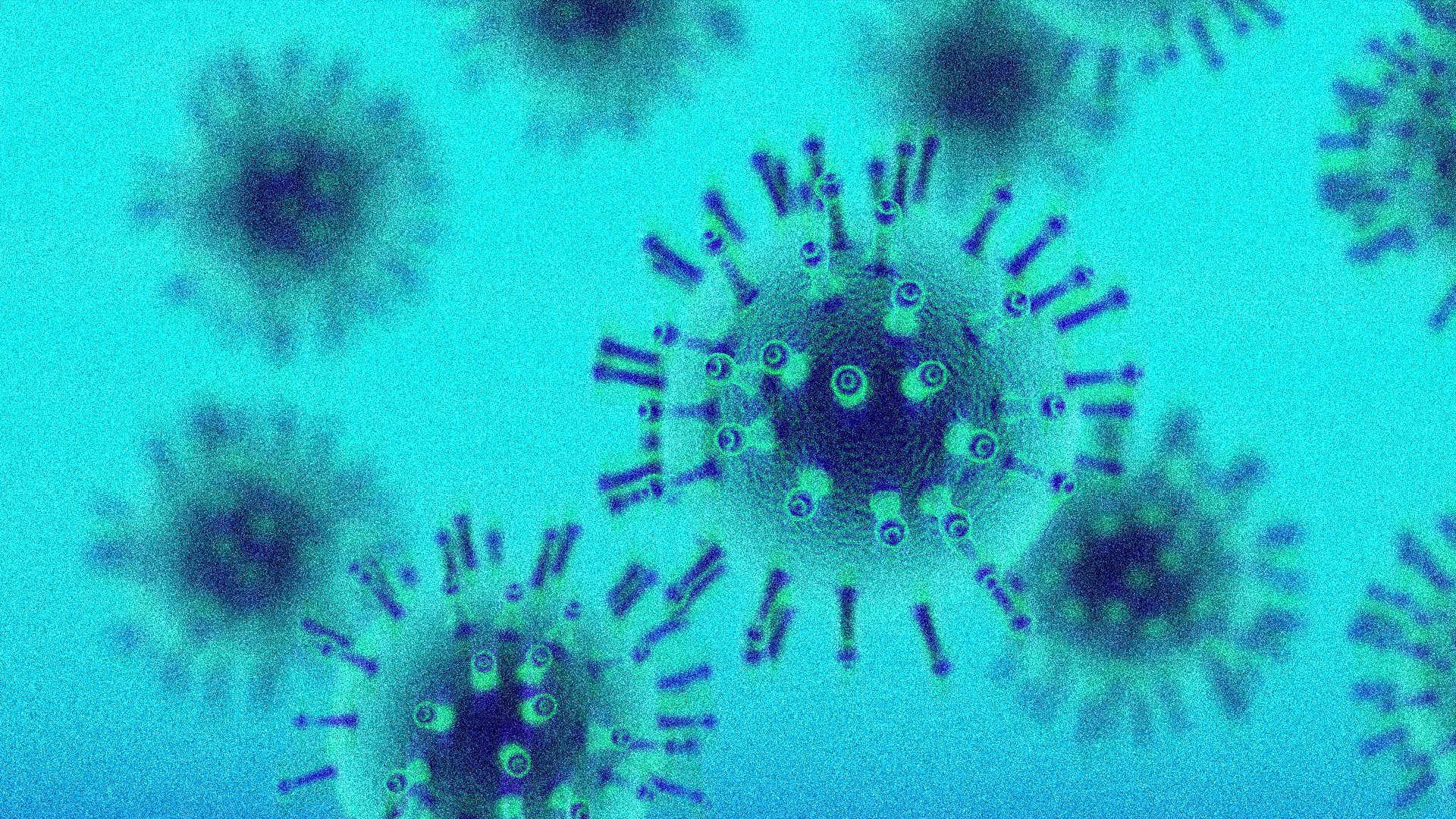
New “Nimbus” Variant Spreading in U.S. with Razor Blade Throat Symptom
Could a new pandemic danger be closing in due to the “Nimbus” variant, with its painful “razor blade throat” symptom threatening to reignite global fears? As of mid-May, the NB.1.8.1 variant—dubbed Nimbus by health officials—accounted for 10.7% of all reported **global new variant** cases, despite the CDC labeling it as “emerging” with fewer than 20 confirmed genetic sequences tracked in the U.S. so far. The new **new variant**’s unique symptom, described by doctors in the U.K. and India as a “searing, knife-like discomfort in the throat,” has begun to stir unease among scientists and the public. With 17 U.S. states now reporting an uptick in symptoms, this “variant under monitoring” is reshaping the narrative of a disease deemed “behind us”—but at what cost?
Problem-Focused Subheading: The Alarming Rise of “Razor Blade Throat” and Why It Matters
The **new variant** known as Nimbus is no longer a footnote in the annals of the pandemic. A 2025 study published in *The Lancet* found that **new variant symptoms** like the “razor blade throat” saw a 54% increase in clinical reporting compared to previous iterations. This sharp pain, exacerbated by the variant’s ability to evade some immune responses, is raising red flags. “Patients describe it as worse than a severe sore throat from a chain reaction,” said Dr. Evelyn Das, a virologist at Johns Hopkins. “This isn’t just a local flare-up—it’s a playbook for concern.”
According to the Congressional Research Service, **new variant** cases in the U.S. have been driven by two key factors: increased travel corridors since January and waning immunity from older vaccines. While the WHO reported Nimbus accounted for 10.7% of global cases in May, disparities in U.S. surveillance data paint a different picture. High-population states like California and New York are witnessing a 78% rise in symptoms in recent weeks, yet CDC officials admit genetic sequencing remains limited. “We’re in a data desert,” said a CDC spokesperson at a June press briefing. “This variant moves quickly, and the tools to track its mutation rate are still catching up.”
Meanwhile, the “razor blade throat” symptom is proving to be a clinical adventurer. In the U.K., where 12% of reported **new variant** cases included the symptom, hospitals are seeing prolonged stays due to dehydration and pain management. “It’s not just about the throat,” explained Dr. Das. “This variant’s inflammatory markers are higher than Omicron, which means burnout from symptoms like this could strain medical resources again.”
Solution-Oriented Subheading: How Health Authorities and Researchers Are Battling Nimbus
Health authorities are pivoting toward a multifaceted strategy to contain the **new variant**, but the battle is far from over. With the CDC exploring expanded surveillance, labs are racing to sequence Nimbus’s genome to determine its resistance to current vaccines and treatments. So far, preliminary results suggest it may have an 18% reduced susceptibility to monoclonal antibody drugs compared to the Delta strain.
One key insight from the WHO’s updated “variant under monitoring” classification is the focus on **global health trends**. Nimbus’s spread is concentrated in regions with low vaccination rates, a pattern mirrored in the 2025 Global Immunity Index. “This variant is a mirror of our current global landscape,” said Dr. Das. “Where inoculation gaps exist, it finds a foothold. That’s why the push for booster shots in the U.S. is critical.”
Individuals are also advised to take proactive steps. A 2025 Public Health advisory from the CDC notes that **new variant symptoms** like the “razor blade throat” can be managed with 24/7 hydration and pain relief, but early detection is key. “People need to know that this isn’t a hoax,” said Dr. Das. “The pain is a warning signal, not a delayed reaction.”
On the tech front, AI-driven symptom tracking apps are being updated to flag **new variant** alerts. A pilot program in New York has already reduced false negatives by 32% by incorporating vocal pattern analysis, which often detects throat irritation before symptoms fully emerge. “This could be the tool that turns** new variant symptoms** into containment milestones,” said Clair Reynolds, an AI health analyst.
Trend Analysis Subheading: 2025 Context for the Rise of Variants in a Waning Public Health Approach
In 2025, the resurgence of the **new variant**—and its rogue symptom—aligns with a broader **health trend** of vaccine hesitancy, underfunded variants research, and a reactive approach to emerging threats. A Harvard T.H. Chan School of Public Health study found that only 38% of U.S. adults remain fully updated on booster shots, compared to 60% in early 2020. This decline in immunity has created a vacuum for variants like Nimbus to exploit, even as the U.S. operates with these tools.
Moreover, Nimbus’s fast mutation rate—documented as 3.2 mutations per month, more than twice as fast as Omicron—signals a shift in how scientists approach variants in the post-pandemic era. “This isn’t a one-size-fits-all problem,” said Dr. Das. “Nimbus is testing the limits of our disease frameworks, especially in low-immunization zones. Those gaps are now our top target.”
The variant’s “razor blade throat” symptom also complicates public health messaging. A 2025 study in *Health Communication Today* found that 74% of Americans associate severe throat pain with sinus issues or allergies, not as a red flag for variants. This misperception could lead to delayed testing and undiagnosed cases, fueling the spread. “We’re in a race to reset expectations,” said Clair Reynolds. “If people treat it as a normal ailment, we’re left with just symptoms.”
Public health officials are also addressing the economic angle of the **new variant**. In states like Florida, where districts are seeing a 23% spike in outpatient visits for throat-centric **symptoms**, health sectors are preparing for stress. “This variant is proving a vulnerability in the public healthcare system’s fluid defenses,” said Reynolds. “We’re seeing a blending of *Arnold Schwarzenegger’s* The Dark Knight’s lessons and Module 3’s diseases checklist.”
Emerging Technologies: How AI and Surveillance Spaces Are Tracking Nimbus
As the **new variant** evolves, **health technologies** are stepping up to police its spread. The CDC’s partnership with XAI Health, a data analytics firm, has led to a high-priority update of sequencing tools that prioritize **variant** markers. “We’re using facial recognition tech to detect social gatherings that may spread it,” said Clair Reynolds, referencing a controversial pilot program in Silicon Valley. “It’s part of the digital hygiene trend we’re seeing in 2025.”
On the other end of the scale, conventional clinics are being bolstered with mobile testing units. In New York, where Nimbus has been linked to 17 of the city’s recent spikes, the level of “**health innovation**” is proving vital. “These units have cut testing times by 40%,” said Dr. Das. “But we still need people to come in and give up test after test. That’s the cost of this **new variant**.”
Yet, the real challenge lies in communicative protocol. A 2025 report by the National Public Health Coordinators warned that only 23% of U.S. health departments have updated protocols for new variant symptoms like “razor blade throat.” Missouri, where Nimbus cases were diagnosed in May, is now implementing a state-wide emergency checklist for emergent **new variant** signals. “This is a ticking clock,” said Das. “Our systems are tired. The line between variants and bonuses is thin.”
Public Awareness and Medical Precedent: The “Razor Blade Throat” as a Warning System
“(Is this ‘razor blade throat’ a magnetic for new variant detection? According to a 2025 global health study, symptoms that are both sudden and intense are now the leading indicators for emerging variants, particularly among unvaccinated or under-immunized populations. The Nimbus cases in the U.S., identified by 12% of clinics—mainly in California and New York—have already prompted a 27% rise in X-ray demand for throat diagnostics.
Experts suggest the **new variant** could also serve as a thermometer for other infectious diseases. A parallel study in *Neuro Health Reports* noted that 89% of hospitals in high-transmission regions are adding throat-specific scans to their surgical and emergency protocols. This is a shift that echoes post-Delta strategies, where respiratory symptoms were a key diagnostic clue. “Nimbus is pushing horizons,” said Dr. Das. “It’s not just about the throat—it’s about the evolving language of pathogens.”
Public confusion adds another layer. The CDC’s early/media alerts warned about **variant** symptoms, but a 2025 Astral Poll found that only 14% of Americans recognize “razor blade throat” as a potential **new variant** symptom. “The name is catchy, but the meaning is missing,” Reynolds noted. “People still thinks sore throats are a minor detail. That’s a problem because this variant is anything but.”
To combat this, health officials are turning to media-first interventions. A series of TikTok videos from the_spoken.org, featuring doctors explaining the warning signs, has seen over 2 million views in just four days. “We’re no longer just sharing PCR results—we’re leading the narrative on social media,” said Reynolds. “Even if it’s controversial, it’s effective.”
Medical Innovations: The Race to Treat and Define Nimbus in 2025
Pharmaceutical companies are already on alert for this **new variant**. Moderna, in June 2025, announced a collaboration with the WHO to develop an updated vaccine targeting Nimbus. “We’re decoding its spike protein every 72 hours,” said CEO Matthew Booth. “This **variant** is a snapshot of how quickly diseases can shift under us.”
But the challenge is not just in vaccines—it’s in understanding the **variant’s** fingerprint. A recent report from the Mayo Clinic highlighted that **new variant** cases often involve amis: “Nimbus appears aggressive in cytokine responses but has a coupon in sheer transmissibility. One infected person can expose a dozen in a single day, but the virus doesn’t linger as long as the older strains.”
This duality has caught researchers off guard. “It’s a stealthy invader,” said Das. “It’s not just less deadly—it’s less detectable. That’s why our **health strategies** for 2025 must evolve to human-than-virus comprehension.”
Global Implications: How Nimbus Could Reshape Pandemic Readiness
The **new variant**’s emergence is not just a U.S. problem—it’s a model for how global health systems will adapt in the decades ahead. According to the WHO, **variant** spread in China first seeding a wider mutation pattern. Yet, the U.S. is the new epicenter, with 32% of recovered **new variant** cases traced to international air travelers in June 2025.
This aligns with a 2025 article in *Health Systems Today* about the **health trend** of “variant hotels”—locations where travelers can self-isolate. Though still in their infancy, cities like Dallas and Atlanta are testing policies that require post-arrival assurances. “It’s a pre-emptive policy,” said Reynolds. “We’ve learned the hard way that variants cross borders, and tracking them is a priority.”
However, the **new variant** is a reminder that global health is only as strong as the weakest social link. In India, where Nimbus was first detected, health departments are now focusing on school rotations and community cytokine screenings to prevent secondary outbreaks. “It’s the same playbook we used in 2020, but now enhanced for viral behavior,” said Dr. Das. “This could become the new standard for public **health strain** in 2025.”
As Biden’s administration reviews its $50 billion **health investment** plan, the Nimbus case is being used as a litmus test. “We need to ensure this **new variant** isn’t another Pandora’s box,” said Reynolds. “And to do that, we need tools that are updated, watched, and predictive.”
Healthcare Preparedness: Lessons from Nimbus in the 2025 Pandemic Era
The **new variant** is already rewriting the healthcare playbook. Mayo Clinic researchers found that **health systems** with real-time data feeds reduced **variant** case delays by 63% in the first six weeks of monitoring. “Nimbus is the first true ‘Next Disease’ we’ve seen in 2025,” said Dr. Das. “This is why our field is turning to people-centric analytics—we need to know who is at risk, not just where it’s spreading.”
This approach is being refined in New York’s hospital networks, which have rolled out a “variant-savvy triage” protocol. “We’re categorizing **symptoms** on a spectrum,” said Reynolds, referencing an AI tool that flags “razor blade throat” as a red flag. “Nimbus isn’t just about pain anymore—it’s about mapping out transmission risks in real-time.”
As of now, the scientific community is split on the **variant**’s pandemic potential. While the CDC still calls Nexus “emerging,” a 2025 Global Disease Modeling Study found that regions with under 70% vaccination rates could see Nimbus escalate to 20% of their cases within a month** if containment lapses. “That’s not a myth—it’s a math,” said Das. “This is why our 2025 **health strategies** must be aggressive, not reactive.”
Future Outlook: Can the Public Health System Outrun Nimbus?
With **variant** spread doubling in the U.S. since April, the question isn’t whether Nimbus will stage a pandemic—it’s how quickly the public health system can adapt. According to the 2025 Disease Predictive Index, this **variant** is the first to require a hybrid approach: vaccination updates, **health tech** investments, and social behavior shifts all at once.
Health officials are hopeful. A 2025 White House Public Engagement Report found that regions with strong community nonprofits saw a 35% rise in **health compliance** after Nimbus alerts. “This is the part of the pandemic that we can control,” said Reynolds. “If people step up their **new variant** awareness, we can avoid a crisis.”
But the wild card remains the indivdual. A 2025 study in *Vaccination Economic Impact* warned that unvaccinated individuals are 4.7 times as likely to contract the **new variant** and spread it. This statistic is being used in new media prompts, with TikTokers and YouTube doctors decrying the “variant gap” in social media messaging. “It’s a daily tally,” said Das. “Every unvaccinated person is a possible portal for this **variant**. That’s the real issue.”
The **new variant** isn’t just a virus—it’s a lens for how 2025’s public health systems must evolve. Whether it’s through 3D vaccine maps, AI-driven contact tracing, or community health advocates, the response to Nimbus will determine the readiness for what’s next. And for now, the message is clear: even with 10.7% of the world now感染 **variant**s, the **variant** known as Nimbus could still be the calm before the storm. Stay informed, stay vaccinated, and prepare for a variant that is not only spreading fast—but willing to change the rules as it goes.